If you’ve ever wished there were easier, safer and far more accessible ways to treat neurological conditions, you’re in for a fascinating ride today. A group of researchers at the Massachusetts Institute of Technology (MIT) has spent the past six years quietly working on something remarkable. Their mission is bold but simple enough to say out loud: take some of the most advanced technologies we have today, blend them together, and create a platform capable of treating a staggering range of neurological diseases and mental health conditions without needing surgery.
Yes, really. No drilling. No electrodes inserted into the brain. No high-risk, high-cost procedures. Instead, this new technology aims to deliver brain implants the same way you’d get a simple injection.
This ambitious system has a name too: Circulatronics. Once you understand what it does, you’ll probably agree that the name fits perfectly.
What Circulatronics Actually Is
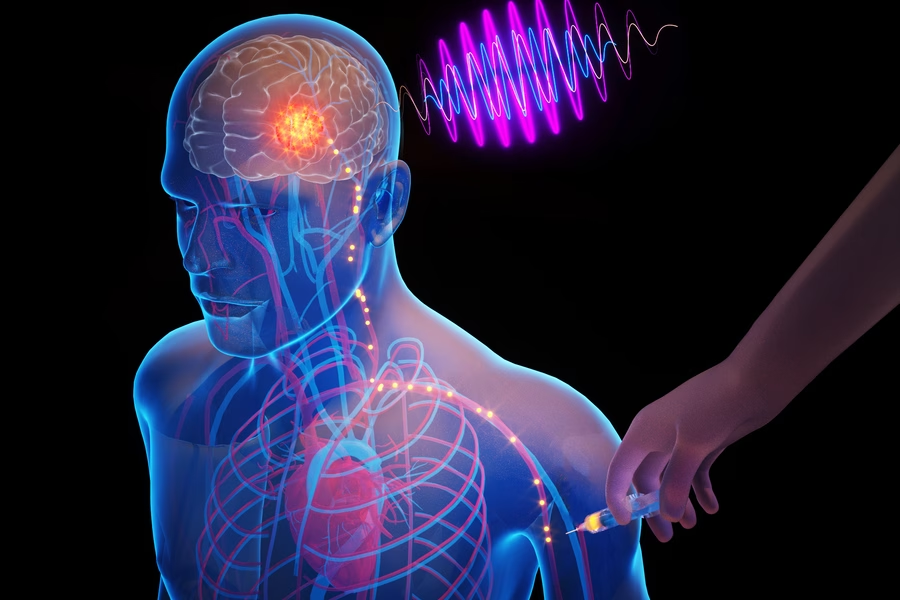
Let’s break down the core idea in the simplest possible way. Circulatronics is designed to combine the power of electronics with the natural transportation systems already inside your body. The goal is to get advanced bioelectronic devices into the brain without surgery, and then activate them to treat neurological issues that affect billions of people around the world.
If that sounds futuristic, you’re right. It is. But it’s also working.
Traditional brain treatments that rely on electrical stimulation require invasive procedures. Surgeons have to open the skull and implant electrodes directly into brain tissue. These surgeries, while often effective, come with a long list of risks including infection, tissue damage and high cost. And for billions of people around the world living with neurological disorders, access to such procedures is simply not possible.
Circulatronics is MIT’s bold answer to all of that.
Why Electrical Brain Stimulation Matters
The entire system revolves around the incredible benefits of targeted electrical stimulation in the brain. Over the past decade, this method has shown promise in treating a wide variety of neurological conditions. It has been explored for depression relief, slowing the effects of Alzheimer’s disease, easing the symptoms of multiple sclerosis and even shrinking brain tumors.
But electrical stimulation only works when the devices are placed very precisely. Until now, the only way to do that has been surgery. Circulatronics flips that requirement on its head. Instead of cutting through bone and tissue to place electrodes manually, this new approach uses microscopic, self-guiding devices that essentially “deliver themselves” to the exact areas that need help.
Imagine receiving cutting-edge brain therapy through a simple injection in your arm. That vision is what this project is making possible.
Meet the Miniature Marvels Behind the System
At the center of the Circulatronics platform are sub-cellular wireless electronic devices, better known as SWEDs. These things are unbelievably tiny. To give you a sense of scale, each one is roughly one-billionth the length of a grain of rice. That is almost inconceivably small, small enough to fit comfortably on a circulating blood cell.
Each SWED is made using organic semiconducting polymers sandwiched between ultra-thin metallic layers. Even though they are microscopic, they still manage to function like ultra-miniaturized brain implants capable of delivering precise electrical stimulation deep within the brain.
Even more impressive is how they’re powered. SWEDs harvest energy wirelessly using a photovoltaic principle—the same basic process used by solar panels. Except here, instead of sunlight, they’re energized by near-infrared light that can pass safely through the skull. A small laser system outside the body activates them, and from there, the devices generate tiny pulses of electricity to modulate brain activity right where it’s needed.
It’s high-tech medicine in one of its purest forms.
How These Tiny Implants Reach the Brain
Creating SWEDs that work inside the brain was only half the challenge. The other challenge was finding a way to get them into the brain safely, precisely and without surgery. This is where a brilliant biological partnership comes in.
Researchers fused each SWED with a living immune cell called a monocyte. These cells naturally circulate through the bloodstream and, most importantly, they can cross the notoriously difficult blood–brain barrier. This barrier is a protective shield that keeps harmful substances out of the brain—but it also blocks most medicines and devices.
Monocytes have one more useful trait: they are drawn to areas of inflammation. And inflammation is a hallmark of many neurological conditions, from Alzheimer’s to stroke. That makes monocytes the perfect biological “delivery vehicle.”
When these monocyte–SWED hybrids are injected into the bloodstream, they navigate through the body, slip into the brain, and automatically home in on inflamed regions. Once they find the target, they implant themselves and settle into place. From that moment on, they’re ready to be activated wirelessly.
What used to require drills, scalpels and hours in an operating room might soon be done with an injection and a guiding push from the body’s own cells.
Putting Circulatronics to the Test
Naturally, the MIT scientists had to make sure this system actually works in living organisms. Their experiments began with mice, and they carried out the testing in two key phases.
First, they needed to prove that the hybrids truly could deliver themselves to specific targets in the brain. To do this, they created a tiny area of inflammation deep inside the mice’s brains, simulating a diseased spot the monocytes would naturally travel toward. Once the hybrids were injected, the team waited 72 hours. After that, they examined the mice and discovered that a significant number of the tiny devices had guided themselves to exactly the right spot.
That alone was a major breakthrough. But the next step was to prove that these self-implanted devices could actually function.
Researchers then shone a near-infrared laser through the skulls of the mice. This activated the SWEDs, prompting them to stimulate nearby neurons. To check whether the neurons had indeed been activated, scientists looked for a protein called c-Fos, which appears in brain cells that have recently been excited.
The results were striking. The treated mice showed a high concentration of activated brain cells—and the activation was extremely targeted, occurring only within a very small area around the inflammation. This precision is exactly what modern brain therapies require.
What This Could Mean for the Future of Medical Care
If Circulatronics continues to succeed as it moves closer to human testing, the impact could be enormous. Imagine treatments for brain cancer, Alzheimer’s disease, chronic pain and other conditions becoming far more accessible, both physically and financially. People who would never be candidates for brain surgery—either due to cost or risk—could receive life-changing therapies through incredibly simple procedures.
And this is just the beginning. The team is already exploring ways to integrate more advanced nanoelectronic circuits into the SWEDs, potentially giving them sensing abilities or even allowing them to act as synthetic neurons.
Another exciting possibility is expanding the technology beyond the brain. Because monocytes can travel throughout the body, these devices could eventually help deliver wireless pacemakers or treat inflammation in other organs.
The scope of potential applications is huge.
When We Might See This in Hospitals
Circulatronics is now on the path toward human trials, thanks to an MIT spinoff company called Cahira Technologies. The hope is to begin clinical trials within the next three years. After that, the technology will still need to navigate regulatory approvals, which will add a few more years to the timeline.
So while it won’t appear in hospitals tomorrow, the progress is real, and the trajectory is promising. If all goes well, Circulatronics could become one of the most transformative medical tools of the coming decade.
For now, it stands as a vivid reminder of how far science has come and how much more is possible when biology and technology work together in ways we never could have imagined.
Source: MIT